Viruses are very different. abide to a set of rules:
Rules of Viruses
- Viruses must replicate to survive.
- Viruses can’t replicate without a host cell.
- All viruses replicate using the same basic steps, but the mechanism varies depending on viral makeup.
- You and another person may take the same route to work, but one of you is using a bicycle and another is using a car.
- Viruses need the machinery of the host cell to replicate.
- And we know that viruses need to replicate to survive.
- If a protein is vital to the survival of the virus, either the virus genome already encodes it or it will use the host’s code. There are no other options. Examples: polymerase and reverse transcriptase
- If it needs something, it’s going to be pre-programmed or you’re going to have it pre-programmed.
- Larger viruses encode non-vital proteins that help the process of replication. Example: herpes scavenging enzymes
- Larger viruses like to encode proteins that help the replication process be more efficient and make less mistakes.
Viruses are weird. They’re so weird that conspiracies are spread claiming they’re not real, not infective, or man-made. On one hand, I’m not surprised I’m seeing this in the depths of the internet in 2018, considering there are full grown adults who genuinely believe the earth is flat. On the other hand, I can understand their confusion and frustration, as the existence of alive-but-not-alive parasites sounds like exaggerated sci-fi. However, unlike the claims I’m seeing in terms of them being “new,” viruses were here long before modern medicine. They’re not a new, they’re just newly observed and evolve over time to become more infective. Centuries ago, one could still diagnose some viral illnesses based off of the similar clinical presentation and characteristic rashes, but even after Leeuwenhoek’s significant contribution to science, you couldn’t whip out a light microscope to directly observe them. The only viruses that can technically be seen with a light microscope are poxviruses. Even then, you’re going off of tiny inclusion bodies and will not have a detailed view.
While viruses are unique from one another in terms of infectivity, antigens, and appearance, they do share many of the same features. All viruses have nucleic acid and a protein coat called a capsid, which protects that nucleic acid so it can survive in the host and replicate. Naked DNA and RNA are highly susceptible to denaturation and degradation in biological systems. RNA is more finicky than DNA since it has that extra reactive hydroxyl group, which is why we don’t use RNA as the main blueprint for our own bodies and need that RNA “middleman” for transcription and translation. A virus gives less shits than the honey badger, though, in terms of reactivity of nucleic acid and comes in all flavors of single-stranded or double-stranded RNA or DNA. A virus still needs to protect its nucleic acids, so it covers it up in that special capsid coat. This capsid comes in multiple different shapes and sizes, and will either be naked or clothed (called enveloped). Counterintuitively, this envelope makes the virus more susceptible to degradation by heat or acid, making enveloped viruses more susceptible to host defense mechanisms and generally weaker in the enteric (gastrointestinal) tract. In other words, while some viruses are stronger than others, enveloped viruses will often be destroyed by the stomach if ingested and have a different route they take for infectivity, such as inhalation or sexual intercourse. It doesn’t mean they’re weak viruses, though. One example would be Human Immunodeficiency Virus, or HIV.
The complete virus particle consisting of the nucleic acid and capsid is called the “virion.”
Viral families often share the same general virion structure. For instance, all alpha, beta, and gamma herpesviruses have a pleomorphic icosahedral capsid consisting of 162 capsomers surrounded by an envelope with embedded glycoproteins:
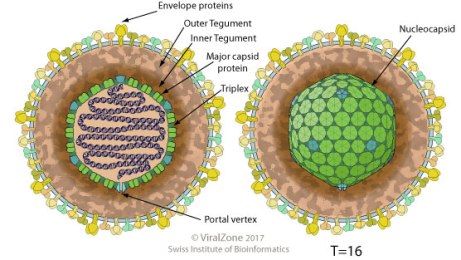
This is just a fancy way of saying that they look the same and they’re built with the same general blueprint (so they are related to one another taxonomically), but they act differently from one another in your body and will be recognized differently. In other words, getting infected with genital herpes HSV2 won’t protect you from getting cold sores via HSV1, as they’re not the same virus. So the differences in each virus comes in outer antigens (they’re recognized as different from one another by your body) and pathogenesis.
All viruses have the same general life cycle inside of a eukaryotic host:
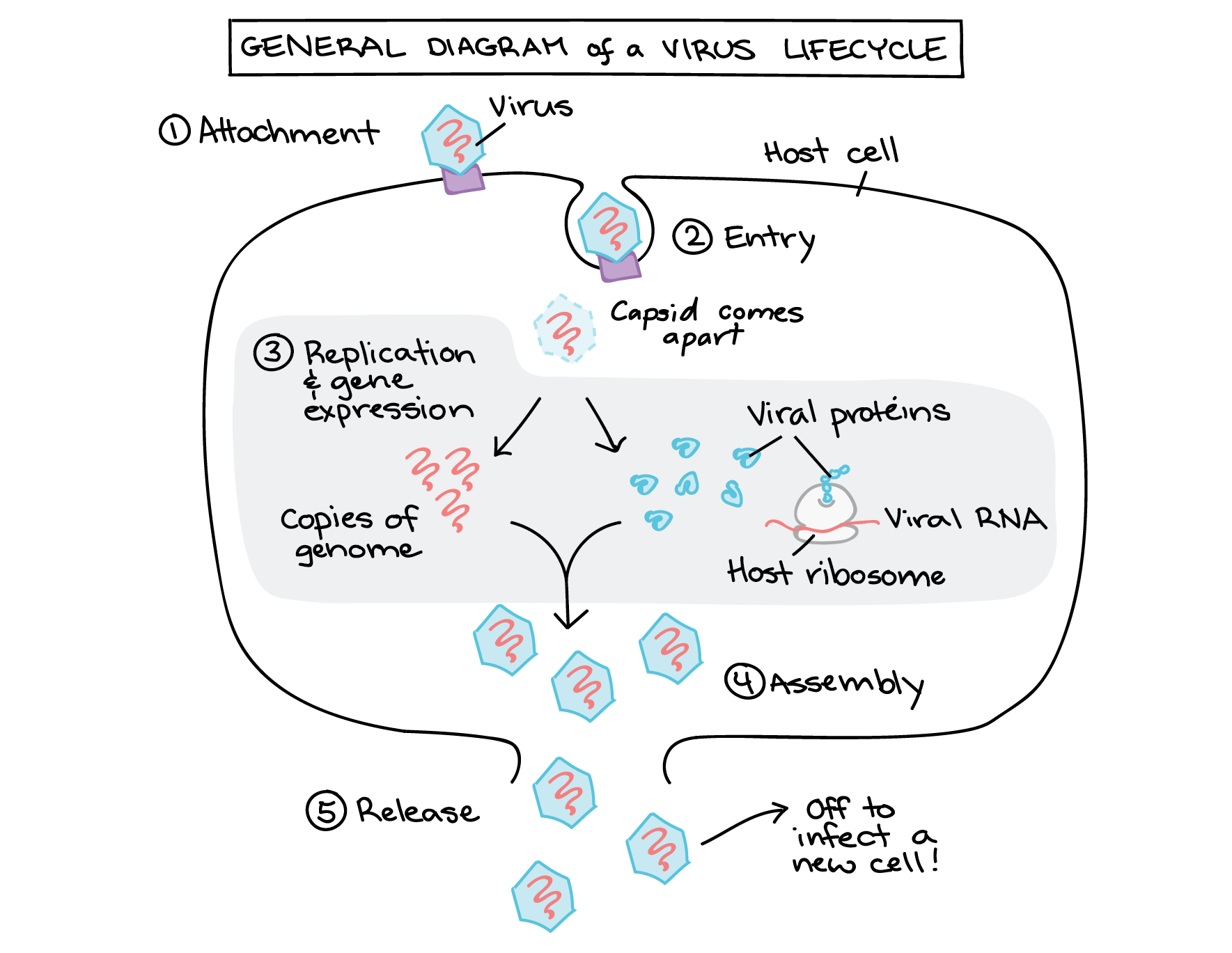
These steps are targeted by antiviral drugs. Of course, the life cycles are a tad more complicated than the general overview shared by all and have a different exit route according to whether or not they have an envelope, which is why one antiviral doesn’t work for every virus (wouldn’t that be nice)
Today we can actually observe viruses infecting cells, incorporating their host genome, packaging proteins, and egress.
Virus packaging materials:
So what viruses do/did we vaccinate against?
1. Smallpox:
Smallpox is the textbook example of vaccine prevention, since we almost completely eradicated it (except for the strains available in labs). What was once a horrible disease now ceases to exist, thanks to the discovery of Edward Jenner.
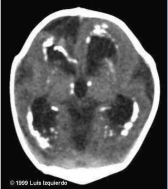
What did it look like?
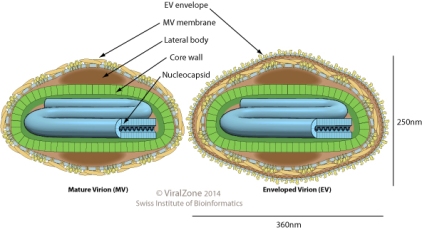
The capsid had complex symmetry, and the overall structure was brick-shaped.
How was it transmitted? respiratory droplets
Pathogenesis and Clinical Presentation:
It multiplied in the throat and then entered the bloodstream where it multiplied further in lymph. About 2 weeks after infection the characteristic rash would appear all over the body in the same stage of development (unlike chickenpox). The spots developed into vesicles and then pustules. The result was that the patient was either dead or scarred.
How does it appear under a microscope? You’d see viral inclusion bodies called Guarnieri bodies that are typical for all poxviruses

How would you diagnose it, then? Both clinical presentation and diagnostic tests testing specifically for the DNA such as ELISA and PCR with western blotting. You would never ever ever ever ever (continued 100x) have a clinical presentation of smallpox without knowing for certain that the person does or doesn’t have smallpox by running specific diagnostic tests. Unless you’re a fan of losing your job and having the entire country hating your guts.
Characteristic rash:


2. Influenza

Pathogen:
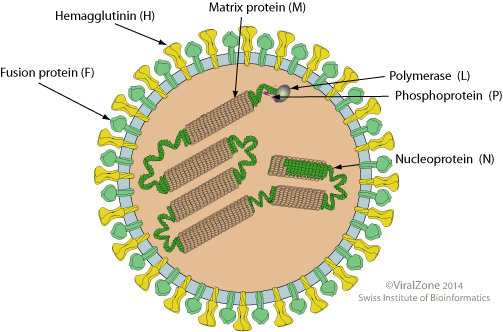
What does it look like?
it’s an enveloped virus with a ssRNA(-) genome. It is pleomorphic with a filamentous capsid

Incubation period: 1-4 days
Spreads via: respiratory droplets
Who is most vulnerable to major complications from influenza? adults >65 and children<5 years, health risks: immunocompromised patients or patients with CVD, diabetes, and seizure disorders
Pathogenesis:
Influenza A: A bad flu – Pandemic influenza
Influenza B: causes epidemics and is usually less serious than influenza A, though children are badly affected. The deaths from influenza B infection often come from myocarditis as well as bacterial pneumonia
Influenza C: Sporadic flu, less serious URI
Antigenic drift → leads to small variations in the surface proteins.
- previous exposure means the person will have partial protection, causing a milder disease.
❍ Antigenic shift → viruses that infect different species infect the same cell and create new viruses during replication with mixed HA and NA antigens.
- Of the three types of influenza virus (types A, B, C), only influenza type A infects multiple species and hence is the only type in which this occurs.
- The different HA and NA antigens are given a number subscript, for example H5N1 (avian influenza, or “bird flu”). These new strains, to which no one is immune at first, are what
cause pandemic flu.
Complications:
- Most who are immunocompetent will be able to fight off influenza.
- Bacterial coinfections of S. aureus (“staph”), S. pneumoniae, S. pyogenes, or H. influenzae occur in approximately 40% – 90% of fatal influenza virus infections.
- encephalopathy,
- transverse myelitis
- Reye syndrome
- myositis,
- myocarditis
- myocardial injury
Signs/Symptoms:
children— Otitis media, nausea, vomiting, and myalgias (usually soleus and gastrocnemius)
Adults and children: abrupt onset of fever, myalgia, headache, malaise, nonproductive cough, sore throat and rhinitis.
How does the influenza vaccine work?
There are two ways in which ρ epitope can be used to improve vaccine development. The first is the development of “like” strains, where the value of p epitope where a similar strain is chosen from several possibilities. It can be used to quantify how close each of the “like” strains is to the desired vaccine strain. This method is difficult, as it is practically impossible to produce in large quantity the exact strain of influenza that is desired for the vaccine, especially in multiple locations across the globe.
The second way in which p epitope can be used is identification of the strains desired to be included in the vaccine. That is, given a list of potential circulating strains, each with probabilities of outbreak for the upcoming year, which vaccine strain minimizes the weighted distance from the potential circulating strains? The value of pepitope can be used to define distance, and so to help choose the closest vaccine strain to the potential circulating strains.
3. Varicella zoster
What does it look like? A typical herpes virus – an enveloped double-stranded DNA virus with icosahedral capsid
How does it spread? Through respiratory droplets and cutaneous lesions. Varicella is a highly contagious, affecting 90% of a family within two weeks if one member gets sick. Community outbreaks usually occur in late winter and early spring months in temperate regions. Unlike chickenpox, Herpes zoster (“shingles”) is nonseasonal. Before vaccination, it was also a common cause of nosocomial outbreaks
Incubation period: averages about 2 weeks – can range from 11-20 days after initial exposure
Pathogenesis:
The virus disseminates into skin and mucous membranes, developing the characteristic lesions. Dissemination may spread to other sites, such as the lungs, in immunocompromised individuals. Adults tend to have more severe clinical presentations compared to children. After infection it remains latent in the posterior dorsal root ganglia.
Clinical presentation:
The rash begins at the scalp and head and spreads to involve the trunk and extremities. Lesions progress through specific stages of erythematous macules, vesicles, pustules, then crusts.
Complications:
Complications in children are common in the immunocompromised. This includes continued lesion development, a very high fever; and visceral involvement. The visceral involvement includes pneumonia (most common complication), meningoencephalitis, and hepatitis.

Adults with a normal immune system typically present with viral pneumonia – a complication that is 25-fold higher than in children. This develops about 1 – 6 days after the onset of rash. Symptoms include:
- cough, shortness of breath, chest pain, and coughing up blood.
Pregnant women also experience pneumonia, and varicella is known to cause spontaneous abortion from fetal demise or birth complications such as growth restriction and musculoskeletal abnormalities


.

4. Rubella
What does it look like?
It’s an enveloped virus of the togaviridae family with +ssRNA

How does it spread? Through respiratory droplets
Pathogenesis and clinical presentation: Patients present with a rash and arthritis

It is a known ToRCHeS infection – it is teratogenic, which means it crosses the placenta and causes fetal damage.
 If the fetus survives, a neonate with congenital rubella will present with the characteristic cataracts, blindness, deafness (most common), thrombocytopenia, heart defects, hepatosplenomegaly, and skeletal deformities. There will also be a large amount of IgM in cord blood. The childhood presentation often consists of a fever with lymphadenopathy and rash and sometimes a secondary spread to CNS consisting of progressive rubella panencephalitis. In adults it may present with post-infectious encephalomyelitis and optic neuritis, myelitis, Guillain Barre syndrome.
If the fetus survives, a neonate with congenital rubella will present with the characteristic cataracts, blindness, deafness (most common), thrombocytopenia, heart defects, hepatosplenomegaly, and skeletal deformities. There will also be a large amount of IgM in cord blood. The childhood presentation often consists of a fever with lymphadenopathy and rash and sometimes a secondary spread to CNS consisting of progressive rubella panencephalitis. In adults it may present with post-infectious encephalomyelitis and optic neuritis, myelitis, Guillain Barre syndrome.
5. Measles:
What does it look like:
It’s a ssRNA(-) virus of the paramyxoviridae family
How does it affect people?
The measles is the hallmark “it’s just a childhood illness” of anti-vaxxers. They’ll continue to defend their “childhood illness” because it makes them feel less shitty for being personally responsible for every outbreak since the vaccine was introduced.
Them: “Oh yeah, well you vaxxers shed!”
Except vaccinated kids don’t shed the measles. If anti-vaxxers ever stopped to read the vaccine inserts (they never do) rather than talking about it, they would know that the MMR vaccine insert is about 20 pages, not a screenshot downloaded from some crunchy granola site, and specifically states that it doesn’t shed. Whoops!
Them: “Well MMR doesn’t protect very long”
It actually protects for a long time, and anyone can get a booster if they’re concerned. Anti-vaxxers seem to be convinced that no one gets boosters. We do. And MMR is efficient.
The measles vaccine alone saved 15.6 million lives annually worldwide annually from 2000-2013. Think one vaccine can’t make a difference ? Think otherwise. Just one vaccine saved many lives in Maputo: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2486532/
Most importantly, it’s not “just a childhood illness,” it’s extremely contagious and deadly. Japan discovered this the hard way. After taking MMR out of the required childhood vaccines, Japan had 200,000 cases of the measles and 88 deaths in just the year 2000 alone: http://www.thelancet.com/journals/lancet/article/PIIS0140673604167159/fulltext
This fit in perfectly with expectations from older peer reviewed science where they first started noticing a trend: https://www.med.nagoya-u.ac.jp/medlib/nagoya_j_med_sci/5514/v55n14p23_32.pdf). Herd immunity is determined via math, so it’s not surprising that they could predict a trend. Japan has been so affected by the measles that they lost a reported $404 million to measles treatment in comparison to vaccination, which costs $165 million https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217873/ Normally it costs the government money to vaccinate (I get mine for free), but not paying for so many measles-induced hospitalizations would had saved them hundreds of millions of dollars. And it was all for nothing. Regardless of fear-mongering, the autism rate in Japan continued to rise as MMR went down: http://onlinelibrary.wiley.com/doi/10.1111/j.1469-7610.2005.01425.x/abstract
Another common antivaxxer myth:
Measles can be cured with Vitamin A!” (e.g “No doctor wants to tell you…”)
Vitamin A can potentially help shorten the duration of the illness and even stop measles progression in many circumstances, and this isn’t some special secret. I’ve never met a single doctor who was “anti-vitamin A.”
Here are the problems:
- Why expose yourself to the measles toxin when we have a safe way to prevent it?
- Taking copious amounts of vitamin A is toxic, as it’s a fat soluble vitamin. This can lead to cerebral edema and liver damage.
- It still doesn’t mean you’re safe. Vitamin A isn’t a cure, but it is recommended for those who have just been diagnosed.
Personally, I prefer prevention rather than simply tossing drugs at people, as anti-vaxxers seem to prefer. Overall, vitamin A can aid in the progression of measles as any healthcare professional will tell you, but it is not a “proven cure,” and is a fat-soluble vitamin, meaning you don’t simply excrete it in the urine like you would with vitamin C. It can be toxic. Someone giving their child a ton of vitamin A in attempts to cure their measles without the help of a medical professional could subsequently kill them. It makes a lot more sense to simply not get the measles and also not contribute to increasing cases of the measles.
“But if Vitamin A helps the measles, that means the measles is a nutritional deficiency!”
This seems to be a popular idea among those who are anti-Germ Theory (I still laugh typing that out). That’s not how the immune system works. Eating healthy and exercising can help your immune system function well, but it’s not a cure. Any doctor out there will ask their patients to eat healthy and exercise. This isn’t a secret either. Back in the “good old days,” we didn’t have processed food. Think about the logic there if it’s supposedly a nutritional deficiency.
Anti-vaxxers: “Well, it’s so rare in the United States it’s not like my child is at risk anyways!”
Your unvaccinated special snowflake is actually 35x more likely to contract the measles compared to their vaccinated friends. When measles was prevalent in the pre-vaccine era, most people experienced infection by the age of 20, and 90% of these reported cases were seen in those kids younger than 10 years old. Your child is highly at risk of contracting the measles.
So how does it spread so easily? It spreads through small-particle aerosols and, unlike many other viruses, can remain infectious for several hours at low relative humidity. It has caused secondary infections in the absence of face-to-face contact with an index case.
Incubation period: about 9-14 days (may be longer in adults)
Fatality: Lower in developed countries and as high as 25% in some developing countries. Most of these deaths result from respiratory tract involvement and/or neurologic complications.
Pathogenesis and Clinical presentation:
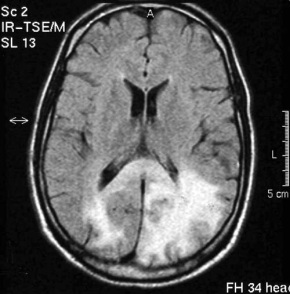
Spreads through the respiratory tract and consists of two stages: Viremic and a second phase of viremia that’s either prodromal or involves dissemination. The disseminated phase can involve the respiratory tract, gut, bile duct, and bladder and spread to lymphoid organs. The typical measles virus–induced giant cells may be present in the tonsils, appendix, other lymphoid organs, and various epithelial surfaces, including those of the respiratory tract. In a typical case, symptoms start similar to a cold. Photophobia (sensitivity to light) usually develops by the second day. Soon, Koplik’s spots develop, small ~2mm macules with a central white dot, will be found around the area of the parotid duct. By the fourth day, these are usually gone and an erythematous rash develops behind the ears. This becomes maculopapular and spreads from the face down the body over the trunk and libs. The fever will increase. The person will typically get better a few days later, but a slew of complications can develop such as an ear infection, pneumonia, encephalitis, subacute sclerosing pan-encephalitis (SSPE- a horrible progressive inflammation in the brain), diabetes, and thrombocytopenic purpura. The most common cause of death in young children is from the measles is pneumonia, which affects about 1/20 of those who contract it. 1/1000 develop SSPE, especially in cases involving younger children. For every 1,000 children who get the measles, 1-2 will die. What can help the measles? Vaccination. Before vaccination, there were about 50 cases of SSPE annually. Now there are only 1 or 2 cases annually.

Important facts about the measles:
- As many as one out of every 20 children with measles gets pneumonia, the most common cause of death from measles in young children.
- About one child out of every 1,000 who get measles will develop encephalitis (swelling of the brain) that can lead to convulsions and can leave the child deaf or with intellectual disability.
- For every 1,000 children who get measles, one or two will die from it.
Information sources:
- Dabbs, David J. Diagnostic Immunohistochemistry: Theranostic and Genomic Applications. Elsevier, 2019
- Dukes, M N. G, and Jeffrey Aronson. Meyler’s Side Effects of Drugs: The International Encyclopedia of Adverse Drug Reactions and Interactions. 16th ed., Elsevier Science, 2015.
- Farizo KM, Cochi SL, Zell ER, et al: Epidemiological features of pertussis in the United States, 1980-1989. Clin Infect Dis 1992; 14: pp. 708-719
- Goljan, Edward F. Pathology. Saunders/Elsevier, 2014.
- Kellerman, Rick D., et al. Conn’s Current Therapy 2018. Elsevier, 2018.
- Robbins, Stanley L., et al. Pathologic Basis of Disease. Saunders Elsevier, 2015.
Image sources:
- http://bacteriologynotes.com/habitat-and-morphology-of-corynebacterium-diphtheriae/
- https://sonoworld.com/Fetus/Case.aspx?CaseId=604&answer=1
- http://bacteriologynotes.com/laboratory-diagnosis-treatment-and-prevention-of-corynebacterium-diphtheriae/
- Diphtheria ECG
-
Case Study: Faucial Diphtheria Complicated with Myocarditis and …
- https://www.visual-science.com/projects/science
- Oleksiy Maksymenko, Getty Images
- https://hoool.com/an-overview-of-strep-throat/http://jvi.asm.org/content/86/23/12571/F2.expansion.html
- http://varicellas.com/2015/03/page/30/
- Sketchymedicine.com
- https://microbiologyinfo.com/differences-between-chickenpox-and-smallpox/
- http://tryptopham.sodoto.net/emrash/
- McKinley et al. 1999 Nontraumatic Spinal Cord Injury: Incidence, Epidemiology, and Functional Outcome
- https://www.sciencesource.com/archive/Bordetella-pertussis–SEM-SS2576968.html
- https://sonoworld.com/fetus/page.aspx?id=153
- http://www.cmaj.ca/content/168/5/561?utm_source=TrendMD&utm_medium=cpc&utm_campaign=CMAJ_TrendMD_1
