Part 3 is specifically made for Tristan Wells, angry Australian protestor against vaccination and Germ Theory who may or may not have the IQ of a humpback whale.
Normally I’d feel bad for singling out someone on the internet, but I can’t quite express how communicating with him feels somewhat like talking to a very angry brick wall. Mistakes were made. Here is an excerpt from his blog on how to debate a pro-vaxxer:
I know what you’re thinking. “Oh come on, he’s trolling.”
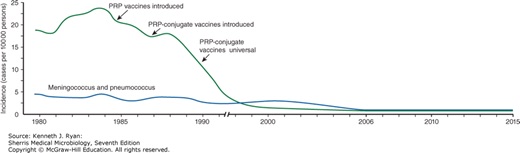
He isn’t. He’s serious. He doesn’t believe in Germ Theory in 2018 and thinks all diseases (I don’t know what he thinks diseases come from either) are renamed. Not just confused with other conditions back in ancient times (which is plausible), or differential diagnoses (which is taken into consideration and part of every patient’s paperwork), but secretly renamed other conditions to convince the world that vaccines work. Welcome to anti-vaxx nutville 2018.
Here is why we’re not “renaming” organisms:
Pathogens have been structurally observed and drawn out. Even if you can’t directly observe it, the body will still create monoclonal antibodies against that organism specifically, not against an organism that has a similar clinical presentation. Vaccine preventable diseases, tetanus being the exception, are not diagnosed by presentation alone but serology, cell culture, or anther specific diagnostic test. Tetanus is the exception because only a few organisms are needed to initiate an infection and they’re obligate anaerobes (exposure to O2 will kill them), making it extremely difficult to isolate. And also because it’s really fucking obvious if patient has lockjaw.
If meningitis, pneumonia, and sepsis were being renamed, it’s amazing how S. pneumoniae is blatantly mentioned in all of my board prep material as the most common cause of community acquired pneumonia and H. influenzae the most common cause of acute epiglottitis. Whenever he’s trying to argue (I’ve had the pleasure of accidentally talking to him once on twitter), he always says what doctors do and don’t do for differential diagnoses, and is wrong every time. He will flip out when you tell him that’s not how it works. He’s convinced that doctors will ignore signs and symptoms of a vaccine preventable disease in vaccinated individuals, which isn’t even close to what actually happens. Signs and symptoms means just that: signs and symptoms. On top of it, we’re obviously not going to have someone’s entire vaccine history in a hospital, but we’ll add it to a SOAP note if they’re not actively dying and we can ask them in person. Pneumococcal pneumonia and Hib are still up there as expected diagnoses of CAP and meningitis. Sepsis can be caused by many different organisms such as E. coli, and they’re going to test for it. If someone who is young and vaccinated comes in with signs of pneumonia and doesn’t have to be admitted, do you know what we treat them for? You guessed it. Without testing, we automatically assume it’s S. pneumoniae and treat them with macrolides. We are more likely to assume S. pneumoniae than whatever other infection Tristan is thinking we’re trying to secretly sell (or whatever he thinks we’re doing), even though he also somehow simultaneously doesn’t believe in Germ Theory.
Fifth Disease vs. Rubeola (measles) vs. Roseola (and I’ll even throw in HFM for free!)
Parvovirus B19 (fifth disease)
|
Virus |
Genome |
Disease |
Transmission/Dx |
Tx/Vaccine |
Comment |
|
Parvovirus B19 (fifth disease) (Erythema infectiosum) |
ssDNA naked linear |
1/5 childhood rashes; must infect replicating cells (erythroid) |
trasmission: oral, respiratory droplets; Dx: IgM IgG serology; PCR for DNA |
no antivirals available; vaccine available for animals only |
most adults sero+; resistant naked capsid; shed virus before symptoms; crosses placenta |
Measles aka Rubeola
|
Virus |
Genome |
Disease |
Transmission/Dx |
Tx/Vaccine |
Comment |
|
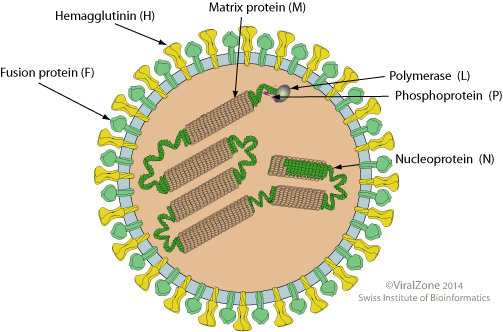
Paramyxoviridae Morbillivirus Measles AKA rubeola |
ssRNA (-) enveloped |
measles -> pneumonia, encephalitis, subacute SSPE, CCC&P; |
aerosols/ Dx: giant cells from fusion |
Vaccine: MMWR (live) Tx: no antiviral |
humans = host; Unique features: maculopapular rash & Kopliks spots; replicate in RT but spreads thru blood -> disease; can spread cell-cell, avoids Abs |
HHV-6 aka Roseola
|
Virus/Family |
Genome |
Disease |
Transmission/Dx |
Tx/Vaccine |
Comment |
|
Herpesveridae Betaherpesviridae Human Herpesvirus 6 AKA Roseola |
dsDNA; enveloped linear |
Appears as prodrome sequence; acute high fever (104 F) followed by classic rash with no other symptoms |
Aerosols, saliva, direct contact |
self-limiting, CMI |
HHV6 also called Roseola or exanthema subitum; rash from activation of Tcells |
Coxsackievirus (not synonymous with HFM, which is a clinical presentation)
|
Virus |
Genome |
Disease |
Transmission/Dx |
Tx/Vaccine |
Comment |
|
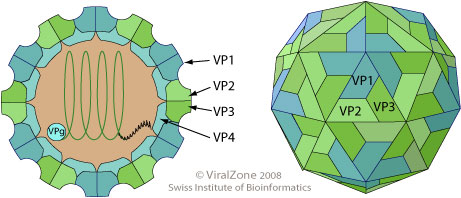
Picornaviridae Coxsackievirus A |
+ssRNA naked |
herpangina; hand foot & mouth; encephalitis, meningitis; carditis, common cold, & more |
fecal-oral Dx: fecal culture; CSF has low neut |
pleconaril if early |
differ strains -> differ disease; infants highest risk; |
|
Picornaviridae Coxsackievirus B |
+ssRNA naked |
pleurodynia, encephalitis, meningitis; carditis, common cold, & more |
fecal-oral Dx: fecal culture; CSF has low neut |
pleconaril if early |
differ strains -> differ disease; infants highest risk; |
Key differences:
- He managed to pick organisms that had completely different nucleic acids from one another. This isn’t like he picked related herpesviruses and asked why we don’t usually get confused – he picked viruses that aren’t remotely similar. All he needs now is a retrovirus and he covered about all of the bases
- HHV-6 will have no other symptoms
- Why would we even “rename” fifth’s with sixth’s disease when neither one of them has a vaccine?
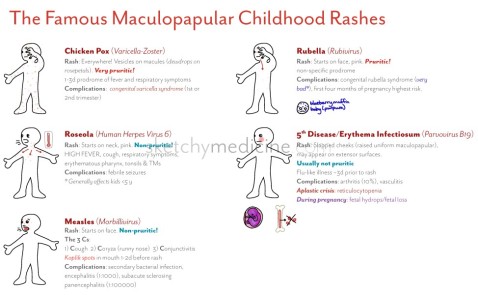
Rashes:
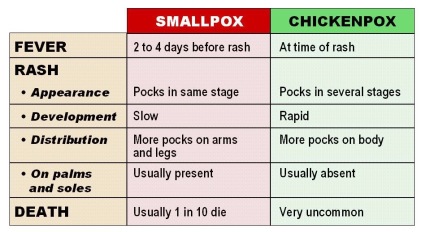
Childhood rashes are distinct from one another.
VARICELLA: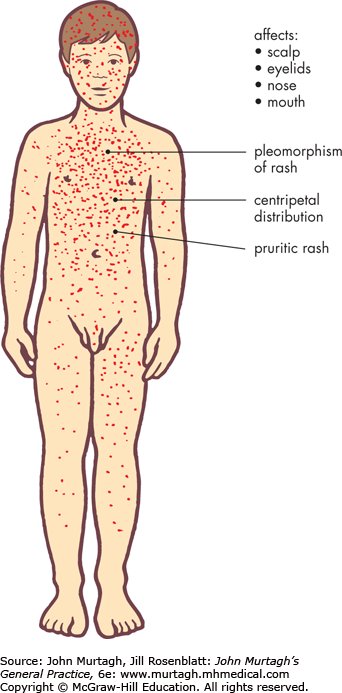
- The pruritic lesions appear in “crops” for about 3-4 days
- The lesions are characteristically described as “dew drop on a rose petal”
- Each lesion is considered contagious until a scab forms
- The “chickenpox” are at different stages of healing
- This sets it apart from smallpox – smallpox will never be at different stages of healing!
-
Spread: From face/trunk to extremities
Duration: ~1 week
ROSEOLA:

- Diffuse, splotchy, maculopapular rash that is NOT pruitic
- This automatically separates it from chickenpox
-
- Rash duration is approximately 24 hours
- Shorter rash duration than the others
- leave no scars — unlike chickenpox
Spread: Very quick – Trunk to extremities and to
entire body
- Rash duration is approximately 24 hours
Strep– This is caused by Streptococcus pyogenes. Strep throat IS tonsillitis caused by S. pyogenes. Tonsillitis can be caused by multiple different organisms. Yes, sometimes including vaccine-preventable diseases. This is why we test patients and include multiple differentials. And yes, tristan, we can easily tell a difference.
The general appearance alone can let someone know they’re dealing with strep or diphtheria. However, patients are still going to be swabbed and tested.


The same goes for pharyngitis and tonsillitis.
Signs and symptoms with variable causes such as pharyngitis and tonsillitis do not determine pathogen upon diagnosis, but rather a disease presentation. To put this in the explain-it-like-im-five version, If you see “-itis,” that means inflammation. So meningitis means an inflammation of the meninges. Pharyngitis is an inflammation of the pharynx, and arthritis is an inflammation of the joints. Some definitions are even more vague, like myalgia. That’s not a disease, that’s a presentation with a slew of different etiologies. That simply means muscle pain. Confusing a pathogen with a presentation is like confusing Van Gogh, the person, with a presentation like impressionism. It doesn’t make an ounce of sense. Streptococcus may be the main etiological agent of pharyngitis, but we still test it if a patient comes in.
Whooping cough vs literally every other cough in existence:
How do we know it’s whooping cough and not a different illness?
For starters: “COUGH COUGH COUGH COUGH COUGH COUGH cough cough cough cough cough cough (x 30) WHOOP” for 100 days kinda gives it away.
The clinical presentation and cough are very specific. The first step in the official diagnosis of pertussis is to have suspicion and proper testing:
- patient with a paroxysmal cough for 14 days or longer and one or more of the following criteria:
- paroxysmal cough, whoop, or posttussive vomiting.
- PCR assay or a confirmed epidemiologic link.
Yes, you are going to be tested for it. Yes, Tristan, even vaccinated kids
Diphtheria can have a variable presentation, so how do we know it’s not a different infection? How do we know it’s not streptococcal or viral pharyngitis or tonsillitis, or Vincent’s angina?
AGAIN: BY TESTING FOR IT!
This information is straight out of my evil Big Pharma class notes–
Diphtheria should be considered in any patient with the following symptoms:
- tonsillitis and/or pharyngitis with pseudomembrane
- hoarseness and stridor
- cervical adenopathy or cervical swelling (bull neck)
- unilateral bloody nasal discharge or paralysis of the palate
Ruled out by culture and isolation
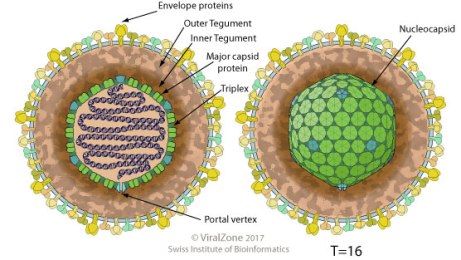
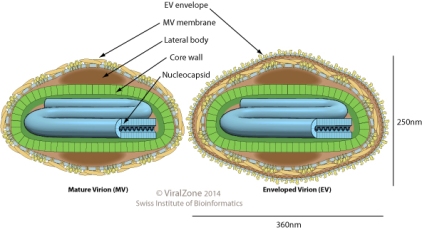
General structure of Herpesviruses:
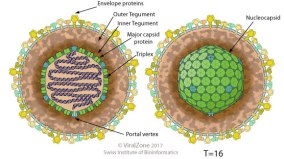
These have similar structure and nucleic acid. This is why they’re in the same family. This doesn’t mean they’re the same disease, this means you wouldn’t diagnose it with an electron microscope (which you wouldn’t do anyways). They have completely different presentations and pathogenesis
vs another DNA virus like:
SMALLPOX
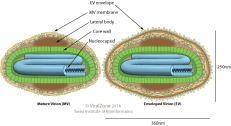
They are a completely different shape, and smallpox is also very large and can technically be seen with a light microscope
Monkeypox vs smallpox-
Smallpox
|
Virus/Family |
Genome |
Disease |
Transmission/Dx |
Tx/Vaccine |
Comment |
|
Poxviridae Smallpox aka Variola |
linear dsDNA |
URT & 2nd viremia->rash; prodromal fever then centrifugal, regular rash |
fomite or lesion/ Guarnieri body |
Vaccine available; VIG 1st; Cidofovir 2nd |
very contagious, can go through skin; humans only host |
Monkeypox
|
Monkeypox poxviridae |
linear dsDNA |
similar to smallpox, reappearing due to vaccinia |
african squirrel-> rodents |
US outbreak 2003 from imported rodents & housepets |
Monkeypox is a zoonotic infection that can appear similar at first to smallpox, which would have scared the living hell out of me if I saw that for the first time. But they’re not the same. Sorry, Tristan. Again, to repeat from Part 2: You diagnose smallpox via both the clinical presentation and diagnostic tests testing specifically for the DNA. You would never ever ever ever ever (continued 100x) have a clinical presentation of smallpox without knowing for certain that the person does or doesn’t have smallpox by running specific diagnostic tests. I have to say this because he’s convinced we don’t add vaccine-preventable diseases as part of our differential. And not only would we, but we would be REALLY FUCKING SURE we weren’t dealing with smallpox. Even if you took the most selfish doctor on earth who didn’t care about their patients, they don’t exactly want smallpox either and would report it to save their own ass and their own literal skin. There is no reason to hide a smallpox diagnosis that wouldn’t result in an immediate firing, a lockdown of a hospital, and a country freaking out. Nothing good would come out of hiding a smallpox diagnosis.


First of all, monkeypox is still extremely rare. Tristan never really explained how so many contracted and died of smallpox every year, and a few people here and there have been affected by monkeypox. Weird… where did they all go? Even if his opinion was true (which we all know it’s not), he still doesn’t explain why there was a sudden drop in smallpox to monkeypox. Wow…. weird.
Monkeypox vs smallpox won’t be diagnosed from observation and biopsy. That’s because both involve a similar morbiliform exanthem. Monkeypox in a clinical presentation that’s milder than smallpox and involves a veroliform rash with progression from papules to vesicles, umbilicated pustules, and crusting. We test it with PCR, ELISA, and/or Western blot. Tristan will say “So? How do you know 100% of smallpox cases were smallpox in the 1600s?” He still doesn’t realize that not only is this a stupid argument (he’s asked this), but it still doesn’t explain how monkeypox was so rampant and where they all went if chickenpox has also dramatically decreased right in front of our fucking eyes right after vaccination was implemented. And it doesn’t explain why we immediately freak out at the idea of smallpox when we’re all in cahoots hiding it under some alternate diagnosis.
Differences: Monkeypox presents with lymphadenopathy and smallpox doesn’t. Also, monkeypox doesn’t transmit the same way as smallpox. Monkeypox is transmitted by typically by contact with infected exotic animal or human-to-human transmission from someone who originally touched an exotic animal. In the United States it’s normally transmitted by prairie dog. Smallpox uh….isn’t exactly transmitted by prairie dogs. I’m not sure if anyone has picked up on that. It’s an extremely rare zoonotic infection. While someone could have easily confused it with smallpox hundreds of years ago, there’s no reason why everyone was getting infected with monkeypox at that time either. It only raises more confusing questions as to what kind of strange things people were doing with prairie dogs and giraffes.
It also doesn’t explain why some cases of monkeypox could be prevented with the smallpox vaccination. They’re similar enough in structure to possibly use one prophylaxis for the other, but how the fuck did it help stop outbreaks if vaccination is all a big giant lie due to to “smallpox being renamed monkeypox?” Magic? It was all renamed chickenpox and …. oh shit, those rates went down too. Tristan will present one giant fail after another.
Smallpox vs severe chicken pox:
Smallpox
|
Virus/Family |
Genome |
Disease |
Transmission/Dx |
Tx/Vaccine |
Comment |
|
Poxviridae Smallpox aka Variola |
linear dsDNA |
URT & 2nd viremia->rash; prodromal fever then centrifugal, regular rash |
fomite or lesion/ Guarnieri body |
Vaccine available; VIG 1st; Cidofovir 2nd |
very contagious, can go through skin; humans only host |
chickenpox-
|
Virus/Family |
Genome |
Disease |
Transmission/Dx |
Tx/Vaccine |
Comment |
|
alphaherpesvirus Varicella |
envelop linear dsDNA |
chickenpox 1/5 childhood rashes |
Aerosol Dx: rash, PCR, culture |
high doses of acyclovir; VZIG-> passive immunity |
More dangerous in adults due to higher chance of pneumonia |
These aren’t even kind of similar, are BOTH VACCINE PREVENTABLE (Hello?) And confusing the two was only an issue before modern medicine. Maybe it’s still confusing to poor Tristan, but to people with basic cognitive functioning, they’re not even close.
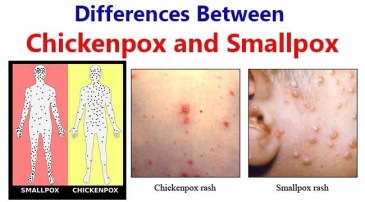 Not the same characteristic rash, not the same clinical presentation, not even the same virus family. In smallpox, lesions begin on the face and then spread outwardly to the extremities, and all lesions will be in the same stage of development. The rash begins at the scalp and head and spreads to involve the trunk and extremities, and the pustules will be at all different stages.
Not the same characteristic rash, not the same clinical presentation, not even the same virus family. In smallpox, lesions begin on the face and then spread outwardly to the extremities, and all lesions will be in the same stage of development. The rash begins at the scalp and head and spreads to involve the trunk and extremities, and the pustules will be at all different stages.
Chickenpox is similar to the same family like HSV, with
Cowdry A or “ground-glass” type inclusions, multinucleated cells, marginated chromatin, and nuclear molding seen under a microscope. Not like smallpox with characteristic Guarnieri bodies.
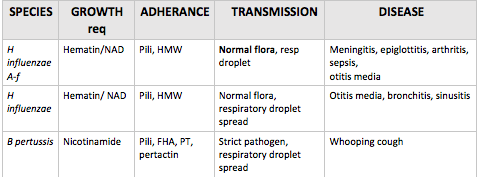
Pertussis vs. H. influenzae
Pertussis and H. influenzae have similar routes of transmission and both cause respiratory infections and otitis media. However, they are also vastly different. Pili is a virulence factor common in gram negative strains that is involved with adhering to host cells, so it’s no surprise that both of them have pili.
Iron lung vs respirator :
This one is the funniest to me. No shit, we use more respirators today. How is that an argument? It would take him seconds to google “how does an iron lung work?” And another six seconds to google “why the flying fuck would someone with more money pay out their ass for an iron lung if it worked the same as a respirator?” If one cost more, anyone with a functioning brain would obviously pick the much smaller respirator over a giant iron lung they had to stay in a majority of the day. And none of this has anything to do with hiding new diagnoses, considering that makes no fucking sense. Yes, we have better technology now. Respirators and iron lungs do not heal people – they help lung function and prolong lives.
COPD – these are the patients using the respirators you’re thinking of. It’s usually from smoking. No, this isn’t secretly polio either, considering we’re STILL TREATING ELDERLY POLIO PATIENTS (sorry) and chronic bronchitis is an obstructive lung condition that comes with specific criteria that doesn’t involve the diaphragm being paralyzed. Yes, Tristan, I’m positive.
Hepatitis vs the alphabet
– The alphabet is not, in fact, hepatitis. Hepatitis is caused by completely different viruses and is named for their affect on the liver. This isn’t rocket science. HepA is normally acute and is in the same family as Coxsackieviridae. HepB is a herpesvirus. HepC is most likely to turn chronic and is in the same family as Rubella. If you’re confused, use the mnemonic “vowels affect bowels”
Guillain-Barre Ddx:
- The paralytic form of rabies shares features with Guillain-Barré syndrome but is clinically distinct because of the presence of myoedema, progression to coma, and urinary incontinence
- Diphtheric polyneuropathy vs Guillain–Barré syndrome (GBS): diptheric polyneuropathy has a slower onset and is more likely to lead to a long term complication or death from diaphragmic paralysis
- You’re way more likely to get Guillain-Barre from a vaccine-preventable disease than a vaccine
Information sources:
- Dabbs, David J. Diagnostic Immunohistochemistry: Theranostic and Genomic Applications. Elsevier, 2019
- Dukes, M N. G, and Jeffrey Aronson. Meyler’s Side Effects of Drugs: The International Encyclopedia of Adverse Drug Reactions and Interactions. 16th ed., Elsevier Science, 2015.
- Farizo KM, Cochi SL, Zell ER, et al: Epidemiological features of pertussis in the United States, 1980-1989. Clin Infect Dis 1992; 14: pp. 708-719
- Goljan, Edward F. Pathology. Saunders/Elsevier, 2014.
- Kellerman, Rick D., et al. Conn’s Current Therapy 2018. Elsevier, 2018.
- Robbins, Stanley L., et al. Pathologic Basis of Disease. Saunders Elsevier, 2015.
Image sources:
- http://bacteriologynotes.com/habitat-and-morphology-of-corynebacterium-diphtheriae/
- http://bacteriologynotes.com/laboratory-diagnosis-treatment-and-prevention-of-corynebacterium-diphtheriae/
- Diphtheria ECG
-
Case Study: Faucial Diphtheria Complicated with Myocarditis and …
- https://www.visual-science.com/projects/science
- Oleksiy Maksymenko, Getty Images
- https://hoool.com/an-overview-of-strep-throat/http://jvi.asm.org/content/86/23/12571/F2.expansion.html
- http://varicellas.com/2015/03/page/30/
- Sketchymedicine.com
- https://microbiologyinfo.com/differences-between-chickenpox-and-smallpox/
- http://tryptopham.sodoto.net/emrash/
- McKinley et al. 1999 Nontraumatic Spinal Cord Injury: Incidence, Epidemiology, and Functional Outcome
- https://www.sciencesource.com/archive/Bordetella-pertussis–SEM-SS2576968.html
- https://www.slideshare.net/Prezi22/rash-illness-training














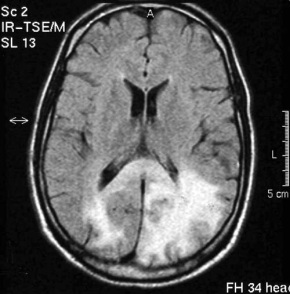
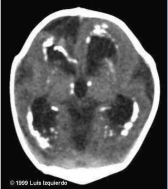 If the fetus survives, a neonate with congenital rubella will present with the characteristic cataracts, blindness, deafness (most common), thrombocytopenia, heart defects, hepatosplenomegaly, and skeletal deformities. There will also be a large amount of IgM in cord blood. The childhood presentation often consists of a fever with lymphadenopathy and rash and sometimes a secondary spread to CNS consisting of progressive rubella panencephalitis. In adults it may present with post-infectious encephalomyelitis and optic neuritis, myelitis, Guillain Barre syndrome.
If the fetus survives, a neonate with congenital rubella will present with the characteristic cataracts, blindness, deafness (most common), thrombocytopenia, heart defects, hepatosplenomegaly, and skeletal deformities. There will also be a large amount of IgM in cord blood. The childhood presentation often consists of a fever with lymphadenopathy and rash and sometimes a secondary spread to CNS consisting of progressive rubella panencephalitis. In adults it may present with post-infectious encephalomyelitis and optic neuritis, myelitis, Guillain Barre syndrome.